By TMoM Team Member Britney Dent
Do you have a child with a rare medical condition? If you don’t, you probably know someone who does.
Before 2020 I had no real idea what a pandemic was and before January 2022 we had never heard of MIS-C. I learned quickly that MIS-C stands for Multisystem Inflammatory Syndrome in Children.
“MIS-C causes different internal and external body parts to become inflamed, including the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal tract. MIS-C can be serious, even deadly, but most children who are diagnosed with this condition get better with medical care.” – CDC
My thoughts: “Why did this happen to my daughter? Will she make it? What are the long-term effects? How will life be different now?
I have three children. My entire household had Covid-19 December 2021, but the children were mostly asymptomatic. We quarantined longer than the recommended number of days, celebrated Christmas on zoom, and canceled all travel plans. By January we were feeling much better, until things took a turn. My daughter woke up one morning and stated that her neck hurt so we alternated ice and heat thinking she “slept wrong”. In the south we call it a “crick in the neck.”
The next day she asked to stay home from school stating she didn’t feel well. My first thought was something was happening at school (a bully, a major test, or bad lunch menu). We let her stay home though this was not her typical request. When she stayed home that day, she stayed in bed and she didn’t get out of bed for two more days besides going to use the bathroom. She didn’t even eat, but she is a baker and aspiring chef!
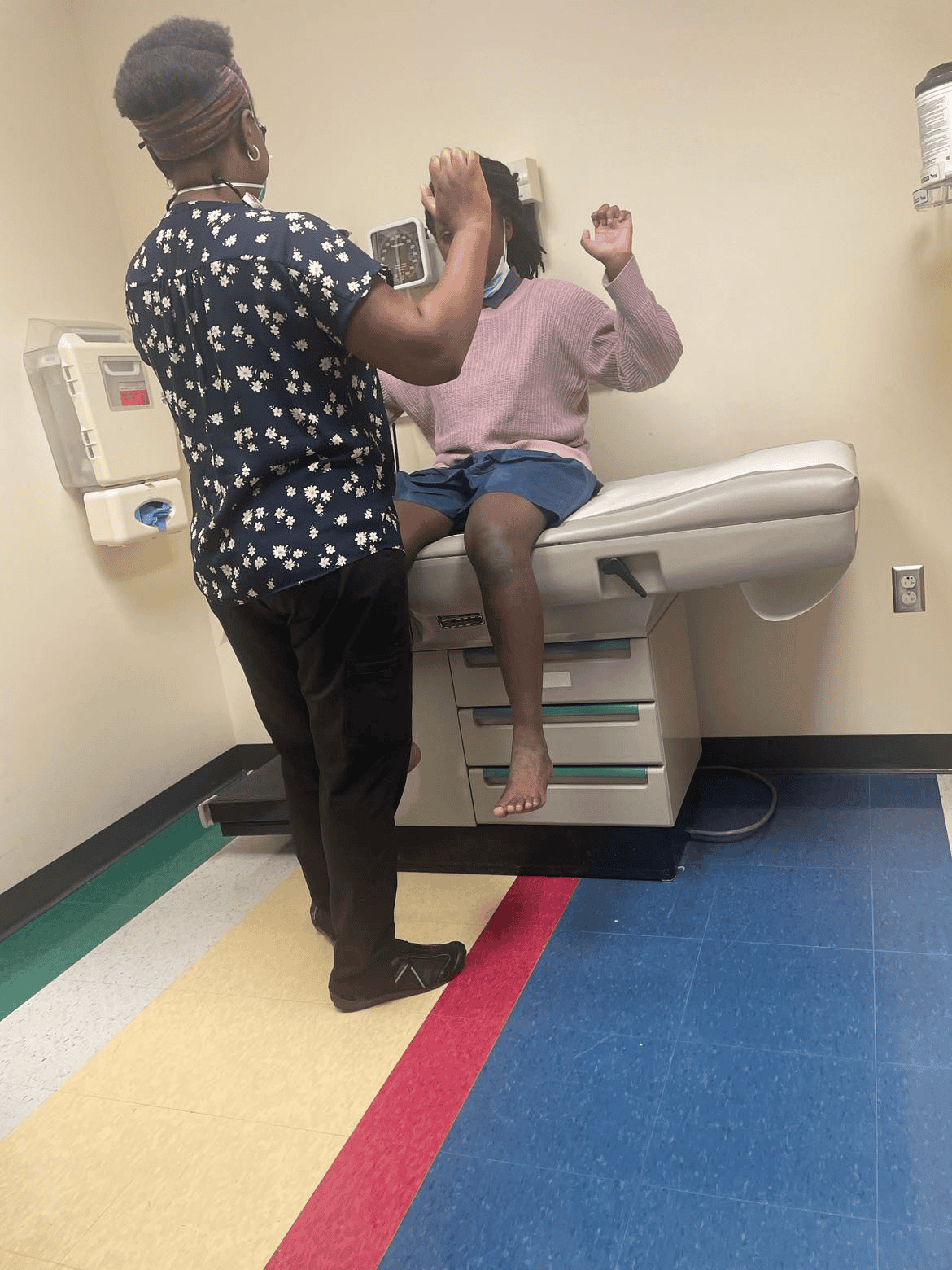
As a family, we decided if she wasn’t better the next day we would take her to the pediatrician to see if she had the flu. I proceeded to go to a doctor’s appointment of my own. While at the doctor, my daughter sent me a text asking to go to the doctor. I rushed home to find that she had experienced fluids leaving her body from both ends, her eyes were bloodshot red, her lips were dry and cracked and she could not walk without falling down. I carried her down three flights of stairs and to the car. On the way to the pediatrician, she continued losing fluids. We arrived at the pediatrician at 4:30 pm. They had decided to squeeze us in before they closed. This was during the time of in car screenings and testing. The nurse came to the car, we rolled down the window and the nurse immediately said: “She needs to go to the ER; she doesn’t look well. Take her to Brenner’s now and we will call and let them know you’re coming.”
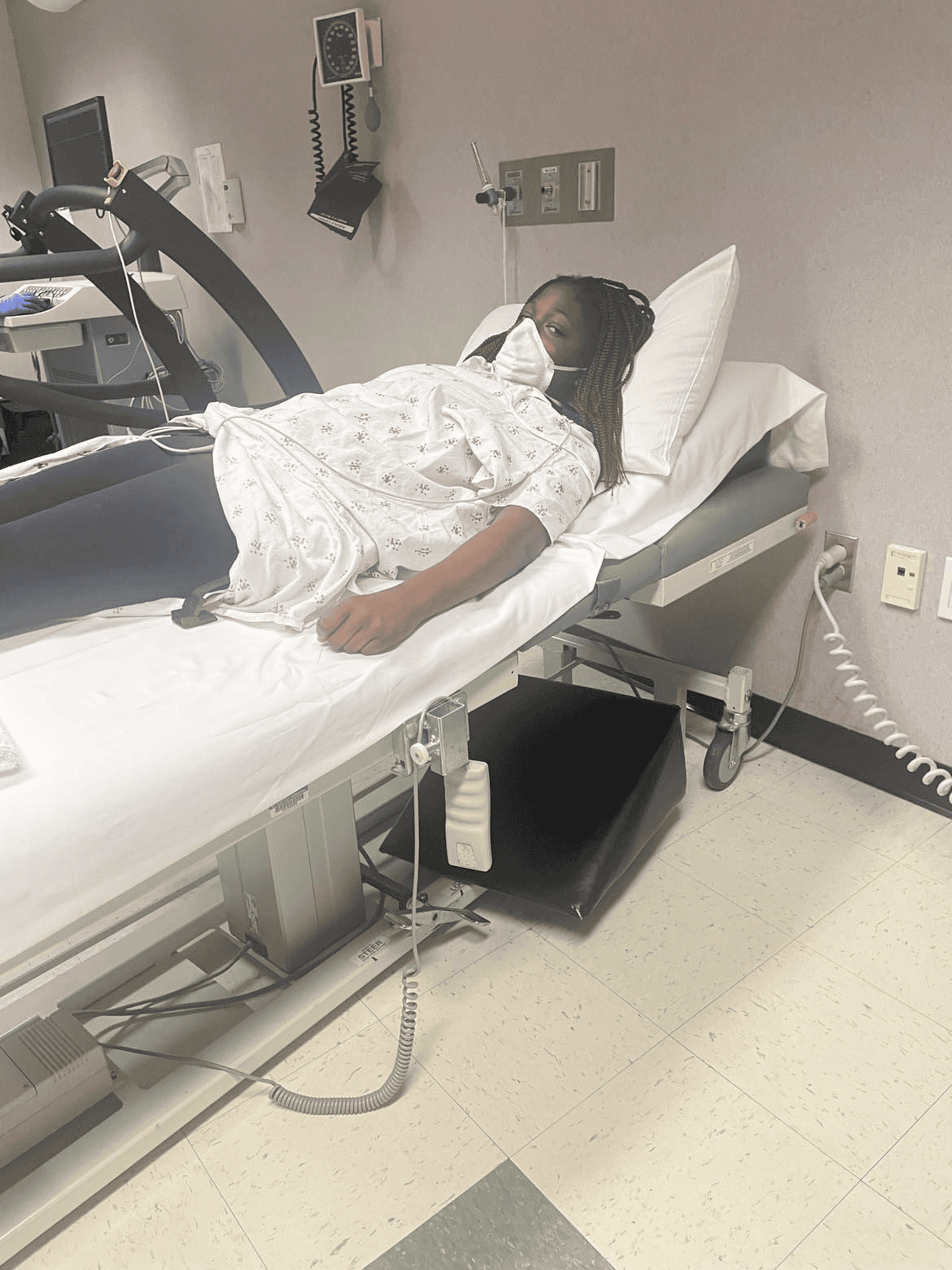
I drive to Brenner’s and thankfully they have valet parking. They bring a wheelchair outside as my daughter is now limp. I wheel her in and they quickly send us back. They hook her to various machines that make a variety of beeping noises and begin asking me a series of questions. My daughter is quickly admitted to the PICU (Pediatric Intensive Care Unit). She stayed there five days before moving to intermediate care.
Why?
Even though our entire household had Covid-19 in December as well as our extended relatives, my daughter was the only one who developed MIS-C. I asked why. Her siblings asked why. She asked why? Doctors did not know why. They still don’t know why.
Will she make it?
Some children with MIS-C also experience shock, which affects blood pressure and heart function. These children require critical care in the Intensive Care Unit (ICU). Although many of the symptoms of MIS-C are similar to those of Kawasaki disease and toxic shock syndrome, MIS-C appears to be a distinct condition. However, medications used to treat Kawasaki disease have also been successfully used to treat MIS-C. We didn’t know during the time of her hospital stay if she would survive but we had faith and hope and a great team of doctors locally that were in constant conversation with children’s hospitals around the world to understand the latest findings for the few children diagnosed with MIS-C.
What are the long-term effects?
Most patients diagnosed with MIS-C recover quickly with treatment. Because this is a newly discovered syndrome, however, the long-term outlook of this condition is still unknown. – Children’s Hospital of Philadelphia
We don’t yet know the long-term effects for my daughter. She has to be monitored annually for the next five years by several practitioners: Cardiologist, Rheumatologist, Physical Therapist, Therapist, Pediatrician, Nephrologist, Radiologist, and Endocrinologist. We are excited to see the data in the years to come of how children with MIS-C have recovered and recouped.
How will life be different now?
Things are back to the “new normal” now and instead of seeing all of those specialists weekly, then monthly, then bi-monthly we have no doctor’s appointments on the calendar until next year!
We still have to list MIS-C on school paperwork, athletic paperwork, camp forms, etc. but we are not sure how life will look down the road. It was a very interesting case too because my daughter was twelve at the time of diagnosis. There are vastly different tests, plans and procedures for children (under 12) and adolescents and adults (over 12). We opted for the children’s procedures to be on the safe side.
Most of the world will not have to deal with MIS-C but if you have to deal with a rare disorder or disease be sure to do the following:
- Advocate for your family member
- Be present for your family member
- Ask questions when you don’t understand
- Remain hopeful
Been there, done that.

Want to see more blogs like this and also get notifications on local events and happenings? Subscribe to our free weekly newsletters here.