Crohn’s Disease: How My Health Crisis Became a Blessing
By TMoM Team Member, Ashley Quinn Kibby
Something was wrong, I could feel it in my gut.
I first began to feel off in the middle of March this year. Anxiety, brain fog, and then the tummy troubles. For a couple weeks I pushed through the pain in my abdomen as I tried to exercise more and eat healthier. All the while I was chasing twin three-year-olds between twenty hours of weekly marketing work. Finally, when the pain began to interfere with my daily routine, I made an appointment with my general practitioner.
My symptoms were common. Gas, bloating, loose stools, and lower abdominal pain. The doctor sent me home with over-the-counter medication and ran some routine bloodwork. It all came back normal. But I didn’t feel normal. I struggled to manage my responsibilities as my health anxiety grew. Soon I could barely move off the heating pad to get to the toilet. When I did, I saw what looked like black tar and blood.
After a visit to the ER, another follow-up with my GP, and additional testing, we learned that several inflammation markers were off the charts. Not only was my abdominal pain insufferable, but I now had blurry vision, joint pain, and a skin rash. Following an urgent colonoscopy which revealed ulcers throughout my small and large intestines, I was diagnosed with the autoimmune disorder Crohn’s Colitis.
I was immediately put on a high dose of Prednisone to control the inflammation. Then the gastroenterologist recommended I start on a class of immunosuppressant drugs called biologics. She told me they’d be given every eight weeks by injection, and I would be on them for the rest of my life. The news about Crohn’s Colitis was devastating. I cried when I heard it. Then I pulled myself together and began my research.
Knowledge is power and introspection is everything.
Over the next few weeks, I frequented Facebook support groups for Crohn’s Disease and Ulcerative Colitis. I learned that biologics like Humira were successful for some, but they weren’t a magic bullet. The process involved trial and error to find the right drug, and the potential for some serious side effects. While these drugs treated symptoms by blocking the immune response, I wanted to understand what my inflammation was trying to tell me. Through my research into alternative medicines, I came to understand that GI issues were often the result of undigested emotional conflict and this idea resonated with me.
Before I got physically ill with Crohn’s Disease, I had been battling anxiety due to chronic stress. While I loved my life beyond measure, I’d been moving through it too quickly and taking too much on with travel, work, and family. The first three years of twin motherhood were the best of my whole life. But they were also the most taxing because I was on constant alert. Plus, I experienced a small identity crisis as many working mothers do. I was compelled by passion and ambition to keep elevating my writing career.
Over these years, I’d begun to take stress-reduction short-cuts, replacing my go-to wellness techniques like yoga, hiking, and dancing with hormone hijackers like cannabis, wine, and junk food. I was really struggling with these cravings and experiencing a lot of cognitive dissonance at the time that I got sick. After processing all this, I began to see my health crisis as an opportunity. Now I had no choice but to treat my body with the love it deserved.
Surrendering to self-care.
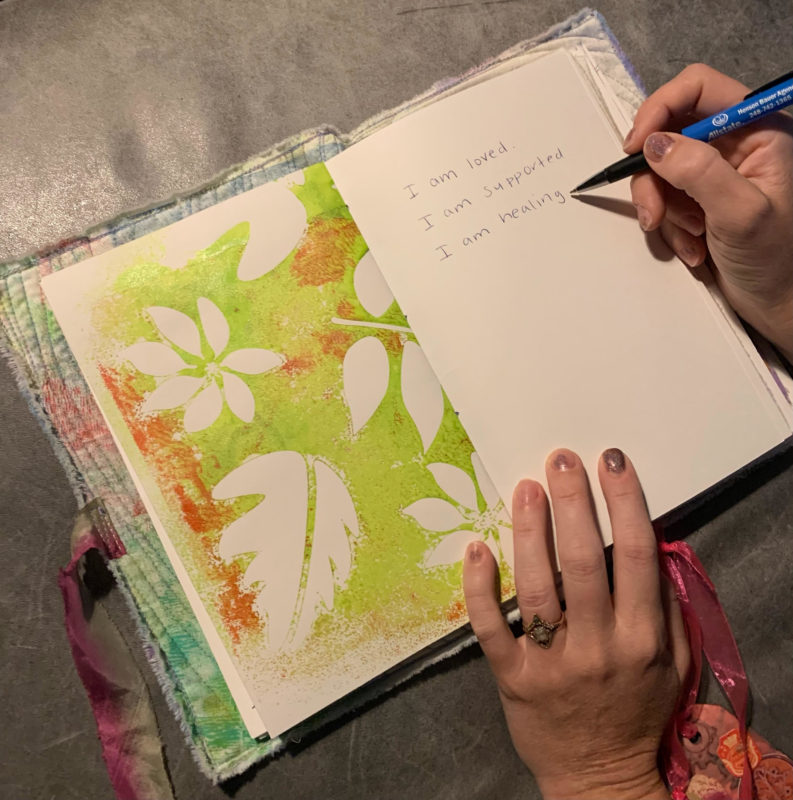
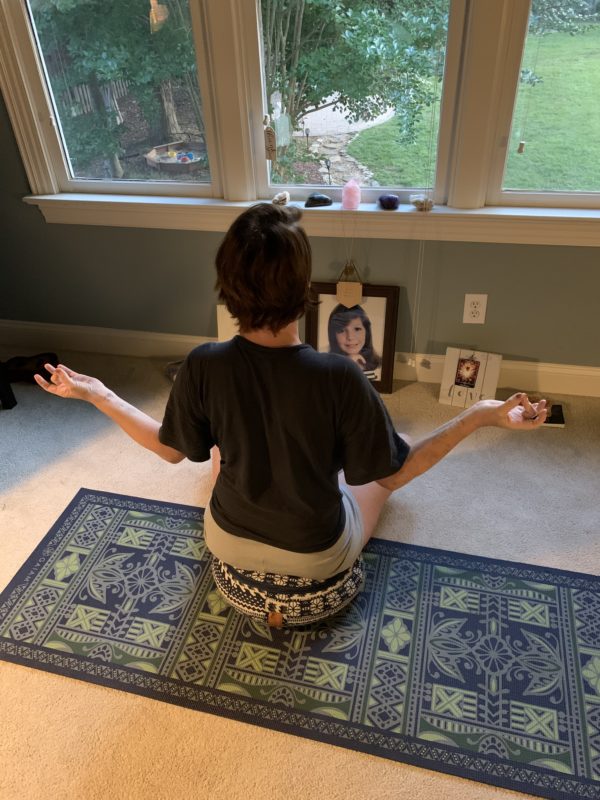
I knew I needed to keep my body in a relaxed or parasympathetic state for healing. Immediately I started with deep breathing, affirmations (I am loved, I am supported), and exercises to stimulate the vagus nerve, which modulates the brain-gut axis.
I told my clients I needed to focus exclusively on my health and felt very fortunate to take a total break from work. I also leaned on my husband and parents for help with meals and childcare. Then I enlisted additional support from health and wellness professionals. I now work with a functional medicine doctor, acupuncturist, and lymphatic therapist.
My functional medicine doctor reviewed all the bloodwork conducted by my GP and advised on nutrition and supplements to heal the gut lining and support my immune system. For a month, I ate only easily digestible foods (chicken, salmon, eggs, banana, avocado, potatoes), twice a day to give my colon a rest. I still avoid dairy, gluten, alcohol, and sugar, and have recently done a GI-MAP test to gather more information to further support my microbiome.

Weekly acupuncture aims to optimize the flow of energy through my digestive organs. Daily lymph work involves self-massage, movement, and breath. I am fortunate to work with an acupuncturist and lymphatic coach who also have Inflammatory Bowel diseases and who have firsthand experience with the emotional-physical stress relationship. Beyond physical modalities, my support team has helped to reinforce mindful practices that serve me throughout the day.
Some great advice I’ve received and put into practice includes…
- Sleep: Regulate circadian rhythms by waking and sleeping with the rising and setting Sun. I now go to sleep before 10pm and wake up at 6am, which allows me time to do self-massage and breathwork before the family wakes up.
- Breath: Start and end the day with a breath practice. One easy exercise is box breathing. Inhale for four seconds, hold for four, exhale for four, hold for four. It’s also great to inhale deeply, pause, and then try to exhale for longer than you inhale. (To learn more about how breath supports the body, I strongly recommend the book Breath: New Science of a Lost Art.)
- Intention: Focus on one project a day and use intention to plan, act, and complete the project. This has helped me tremendously as my tendency was to pack as much in as possible, often jumping from one project to the next before even finishing.
- Inspiration: Exercise your creative outlets for the joy of it. For me, this is writing. My obsession with getting published emphasized validation from external sources over enjoying the flow of my passion.
Finding growth through gratitude and a mindful mindset.
The benefits of these lifestyle and mindset changes have been amazing. I love to wake with the birds and sun and sleep when I’m tired. Each day I aim to be completely present with my girls and husband. I’ve also released the pressure to perform and achieve greatness. There’s nothing like a health crisis to put things in perspective. Restoring the relationship between my mind and body is now my top priority.
After one month of self-care devotion, my GI symptoms had largely subsided, and I was able to taper off the prednisone. Two months following my diagnosis, I continue to have joint pain and vision irregularities that require follow-up with a rheumatologist and ophthalmologist. Still, I see the lingering issues as a reminder to take it slow as I give thanks for the remarkable progress I’ve already made.
While it’s not always easy to focus on the positive when your health suffers, gratitude is a powerful healing force in its own. I am grateful beyond measure for the support of my family and clients. I am grateful that my healing journey began in the Spring, with the Sun inviting me to rise and the forest critters calling me to the trails. (Did you know that walking amongst trees has been clinically proven to lower cortisol levels?). I am also incredibly grateful that the hardest part of caring for twins is behind me in terms of the physical labor of diapers, meals, language barriers, emotional regulation development, and sleepless nights. My girls are a joy, and I am here for it!
I know I am not out of the woods yet with Crohn’s Colitis, and I am not in denial that I am dealing with a lifelong dis-ease and my treatment plan may change over the years. But, for now, I relish the joy of healing. I embrace the discipline of it. Most of all, I marvel at how this horrible situation has transformed into a blessing. Finally, I feel anchored into the present moment and committed to the lifestyle and mindset I have always wanted for myself.

*This article reflects the personal experience of the author and is not medical advice. If you experience symptoms of an illness, please consult your doctor.
Want more great ideas for Parenting in the Triad? Sign up for our free weekly newsletter here!